Understanding Homeostasis: The Body's Balancing Act
Understanding Homeostasis: The Body's Balancing Act
Have you ever wondered how your body manages to stay consistent, even when the world around you is constantly changing? From extreme temperatures to sudden stress, your body's internal environment remains remarkably stable. This remarkable ability is known as homeostasis.
Imagine your body as a finely tuned orchestra. Each instrument plays its part, contributing to a harmonious symphony. But what happens if one instrument goes out of tune? The entire performance suffers. Similarly, your body's internal environment must remain in balance for optimal functioning.
Homeostasis is the body's ability to maintain a stable internal environment, despite external changes. It's essential for survival, as our cells and organs depend on a consistent environment to function optimally. Think of it as the body's built-in thermostat, constantly adjusting to keep things within a healthy range.
Why Does Homeostasis Matter?
1. Optimal Cell Function:

Our cells are delicate and require a specific environment to function properly. Homeostasis ensures that they have the right temperature, pH, nutrient levels, and oxygen supply.
2. Disease Prevention:

When homeostasis is disrupted, it can lead to various health problems. For example, diabetes is a condition characterized by high blood sugar levels due to a deficiency or resistance to insulin. Dehydration occurs when the body loses too much fluid and cannot adequately replenish it.
3. Enhanced Performance:

Homeostasis is crucial for athletes and individuals who engage in physically demanding activities. It ensures that the body can meet the increased demands for energy, oxygen, and waste removal.
4. Stress Resilience:

Homeostasis helps the body cope with stress. When faced with challenges, the body's internal systems work together to maintain balance and promote recovery.
In this blog, we'll delve into the science behind homeostasis, explore examples of its action, and discuss its impact on health. By understanding how our bodies maintain balance, we can appreciate the complexity and beauty of human biology.
Section 1: The Science Behind Homeostasis
Basic Concepts of Homeostasis
At the heart of homeostasis lies the concept of equilibrium, a delicate balancing act that the body constantly strives to maintain. This means that various physiological parameters, such as temperature, pH, blood pressure, and glucose levels, must remain within a specific range for optimal functioning.
Equilibrium: The Foundation of Homeostasis
Think of equilibrium as a tightrope walker. The walker must constantly adjust their balance to stay on the rope. If they lean too far to one side, they risk falling. Similarly, the body must constantly adjust its internal environment to maintain equilibrium.
Physiological Parameters
Temperature:

The body maintains a core temperature of around 37°C (98.6°F). Deviations from this temperature can have serious consequences, such as hypothermia or heatstroke
PH:
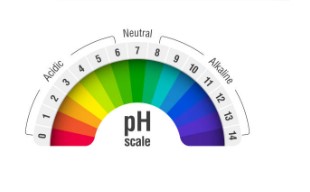
The pH of the blood and other bodily fluids must be carefully regulated. An imbalance in pH can disrupt enzyme activity and affect the function of cells and organs.
Blood Pressure:

Blood pressure is the force exerted by blood against the walls of blood vessels. It must be maintained within a healthy range to ensure adequate blood flow to tissues and organs.
Glucose Levels:
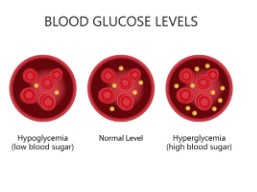
Blood glucose levels are regulated to provide a steady supply of energy to cells. Excessive glucose can lead to diabetes, while low blood sugar can cause hypoglycemia.
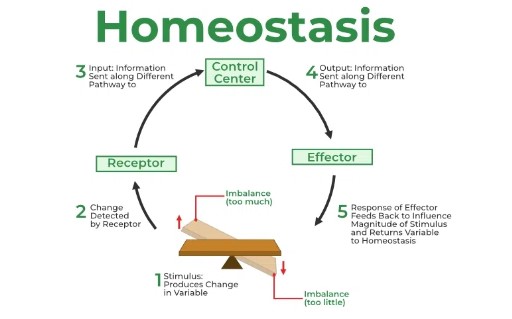
Feedback Mechanisms: The Body's Control Systems
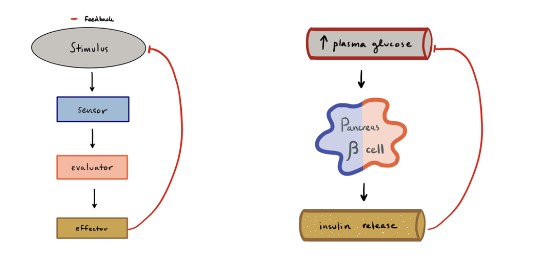
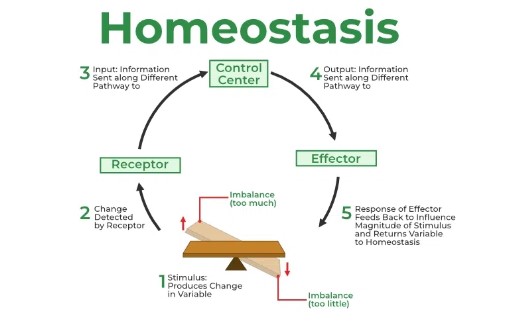
To maintain equilibrium or homeostasis, the body relies on intricate feedback mechanisms that act as built-in control systems. These mechanisms constantly monitor the internal environment, detect deviations from an optimal state, and initiate appropriate responses to restore balance. They are essential for regulating body temperature, blood pressure, glucose levels, and many other vital physiological processes..
Feedback Loops
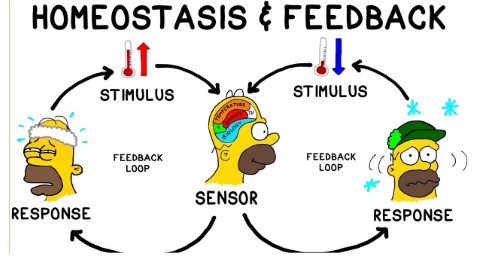
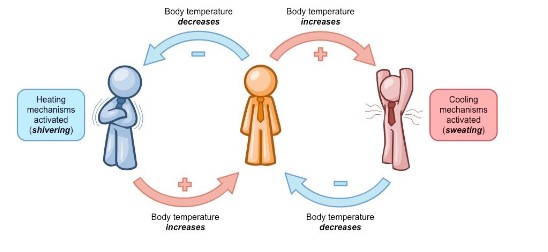
Negative Feedback: The most common type of control system in the body is the negative feedback mechanism. It operates like a thermostat in a home. When a sensor detects that a physiological parameter, such as body temperature or blood sugar, has moved out of the normal range, the body triggers processes to correct it. Once the parameter is back within its set point, the response is halted. For example, consider thermoregulation. When the body temperature rises above the normal range, sensors in the skin and brain detect the increase. The body responds by activating mechanisms such as sweating and vasodilation (the widening of blood vessels), which help release heat and cool the body down. When the temperature returns to normal, sweating and vasodilation stop. Similarly, when body temperature drops, the body activates processes like shivering and vasoconstriction (narrowing of blood vessels) to conserve heat. Another common example of negative feedback is blood sugar regulation. After eating, blood sugar levels rise, prompting the pancreas to release insulin, which helps cells absorb glucose. Once blood sugar levels are reduced to a normal range, insulin secretion decreases.
Positive Feedback: In contrast to negative feedback, positive feedback mechanisms amplify the initial stimulus rather than reversing it. These mechanisms are less common but play critical roles in specific situations, such as childbirth and blood clotting. During childbirth, the release of oxytocin causes contractions of the uterus, which pushes the baby toward the birth canal. As the baby moves, it stretches the cervix, which signals the brain to release more oxytocin, further intensifying contractions. This cycle continues until delivery. Similarly, in blood clotting, when a vessel is damaged, platelets adhere to the site and release chemicals that attract more platelets, forming a clot. This positive feedback loop continues until the bleeding stops.
Negative Feedback: A Closer Look
Negative feedback is the primary mechanism used to maintain homeostasis. Here's a breakdown of how it works:
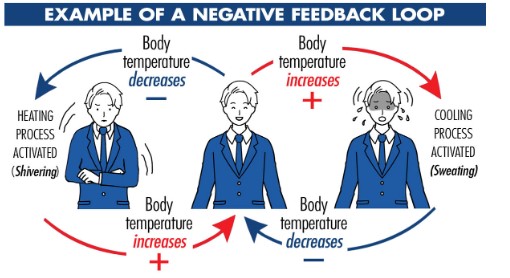
Sensor: A sensor, such as a nerve ending or a specialized cell, detects a change in a physiological parameter.
Control Center: The information from the sensor is sent to a control center, often in the brain or endocrine system.
Effector: The control center analyzes the information and sends a signal to an effector, such as a muscle, gland, or organ.
Response: The effector responds in a way that counteracts the change.
For example, if blood pressure rises above normal, the body responds by activating the baroreceptor reflex. This reflex involves the following steps:
Sensor: Baroreceptors in the carotid arteries and aortic arch detect the increase in blood pressure.
Control Center: The information is sent to the medulla oblongata in the brain.
Effector: The medulla oblongata sends signals to the heart and blood vessels
Response: The heart rate slows down, and blood vessels dilate to reduce blood pressure.
Positive Feedback: A Brief Overview
While less common, positive feedback loops can also play a role in homeostasis. In these loops, a change in a parameter is amplified rather than reversed. This can be beneficial in certain situations, such as childbirth or blood clotting.
During childbirth, for example, the contractions of the uterus stimulate the release of oxytocin, a hormone that further increases uterine contractions. This positive feedback loop helps to expel the baby.
The Role of the Nervous and Endocrine Systems
The nervous and endocrine systems play crucial roles in coordinating homeostatic responses. The nervous system rapidly detects changes and sends signals to effector organs, such as muscles and glands. The endocrine system releases hormones into the bloodstream, which can have widespread effects on the body.
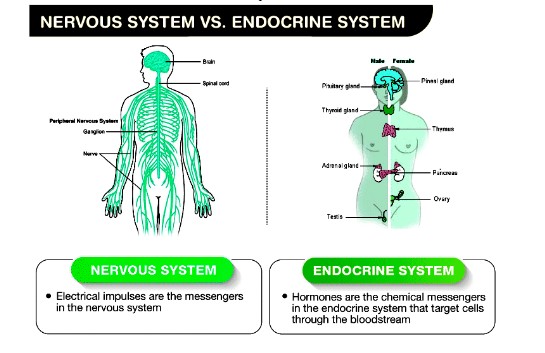
- Nervous System: The nervous system consists of the brain, spinal cord, and peripheral nerves. It receives information from sensors throughout the body, processes the information, and sends signals to effector organs.
- Endocrine System: The endocrine system is composed of glands that produce and secrete hormones. Hormones are chemical messengers that travel through the bloodstream to target organs.
Together, the nervous and endocrine systems work to maintain homeostasis by coordinating the body's response to changes in the internal and external environment.
Importance of Feedback Mechanisms: A Closer Look
The body's feedback mechanisms are critical for survival, allowing it to maintain a stable internal environment, or homeostasis, despite external and internal changes. These mechanisms are complex, highly regulated systems that monitor various physiological parameters such as temperature, blood sugar, and blood pressure. By continuously adjusting these parameters, the body ensures that its internal conditions remain optimal for cellular function, which is crucial for overall health and well-being.
Negative Feedback: The Primary Control System
Negative feedback mechanisms are the most prevalent and significant feedback systems in the body. They work to reverse or reduce deviations from a set point, maintaining a stable state. These systems are essential because most of the body's physiological processes operate within a narrow range. Even slight deviations from this range can lead to dysfunction or disease.
For example, consider the regulation of body temperature. The human body must maintain a core temperature of around 37°C (98.6°F) for enzymes and cellular processes to function correctly. When the body overheats due to external conditions like a hot climate or vigorous exercise, thermoreceptors in the skin and hypothalamus detect the rise in temperature. The brain then signals effectors, such as sweat glands and blood vessels, to initiate cooling mechanisms. Sweating promotes heat loss through evaporation, while vasodilation increases blood flow to the skin, allowing more heat to dissipate. Conversely, when body temperature drops, the hypothalamus triggers shivering (muscle contractions that generate heat) and vasoconstriction (narrowing of blood vessels) to conserve heat. Without this finely tuned negative feedback system, extreme temperatures could lead to hyperthermia (overheating) or hypothermia (excessive cooling), both of which can be life-threatening.
Blood sugar regulation is another classic example of negative feedback. After consuming a meal, blood glucose levels rise, which could be harmful if unregulated. The pancreas detects this increase and releases insulin, a hormone that facilitates the uptake of glucose into cells for energy or storage as glycogen in the liver and muscles. This action lowers blood glucose levels to a normal range. In contrast, when blood sugar levels drop, such as during fasting or prolonged exercise, the pancreas secretes glucagon, which stimulates the liver to release stored glucose into the bloodstream. This constant balancing act prevents conditions like hyperglycemia (high blood sugar) or hypoglycemia (low blood sugar), both of which can have severe consequences, including coma or death if left unchecked.
Positive Feedback: Amplifying Responses in Critical Situations
Unlike negative feedback, which promotes stability, positive feedback mechanisms amplify the initial stimulus to drive a process to completion. While less common, positive feedback plays a crucial role in specific, time-sensitive processes where an amplified response is beneficial.
One of the most well-known examples is childbirth. The process of labor is initiated when the fetus presses against the cervix, triggering the release of oxytocin from the pituitary gland. Oxytocin intensifies uterine contractions, pushing the baby further into the birth canal. This increased pressure stimulates even more oxytocin release, further amplifying contractions. The cycle continues, escalating the intensity of labor until the baby is delivered. Once childbirth is complete, the stimulus (pressure on the cervix) is removed, and the positive feedback loop ceases. Without this mechanism, the process of childbirth would be prolonged and inefficient.
Another example is blood clotting, a critical process that prevents excessive blood loss following injury. When a blood vessel is damaged, platelets adhere to the injury site and release chemicals that attract more platelets. This aggregation forms a clot, which stops the bleeding. The positive feedback loop ensures that the clotting process is quick and localized, preventing further blood loss. Once the injury is sealed, the process halts, avoiding unnecessary clot formation elsewhere in the body, which could lead to dangerous conditions like thrombosis.
The Balance Between Feedback Mechanisms
While both negative and positive feedback mechanisms are essential for health, they operate in different ways and must be carefully regulated to prevent dysfunction. The body primarily relies on negative feedback to maintain homeostasis because its goal is to counteract changes and stabilize the internal environment. Disruption of negative feedback mechanisms can lead to serious health issues. For instance, in diabetes mellitus, the negative feedback system for regulating blood sugar is impaired, resulting in chronically elevated glucose levels, which can damage organs and tissues over time.
In contrast, positive feedback is designed to be self-limiting. It is typically triggered in situations that require an all-or-nothing response. Positive feedback loops, if not properly controlled, can lead to pathological conditions. For example, in cases of sepsis, an unchecked immune response triggers a positive feedback loop that leads to widespread inflammation and tissue damage, potentially resulting in organ failure or death.
Conclusion
In summary, feedback mechanisms are fundamental to the body's ability to adapt to changing conditions and maintain internal balance. Negative feedback systems dominate because they provide the stability required for most physiological functions, preventing excessive fluctuations that could lead to disease. Positive feedback systems, although less common, play vital roles in driving processes to completion, particularly in emergencies or during critical events like childbirth and blood clotting. Together, these feedback systems ensure that the body can maintain homeostasis and respond effectively to both internal and external challenges, supporting health and survival.
Section 2: Examples of Homeostasis in Action

Homeostasis is a complex process that involves multiple physiological systems working together. Let's explore three key examples: temperature regulation, blood sugar control, and fluid balance.
Temperature Regulation
One of the most familiar examples of homeostasis is temperature regulation. The body maintains a core temperature of around 37°C (98.6°F). This temperature is essential for optimal metabolic processes.
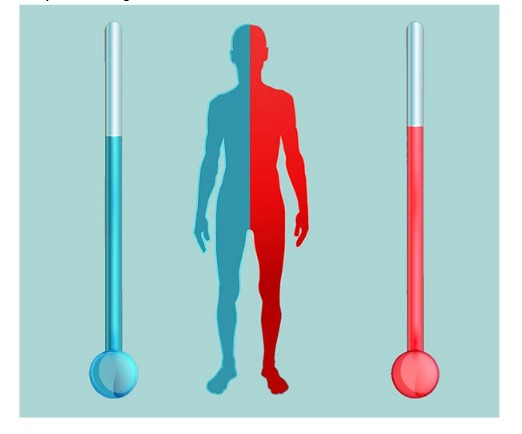
To regulate temperature, the body uses a variety of mechanisms:
- Vasodilation and Vasoconstriction: When the body is too hot, blood vessels near the skin dilate (vasodilation) to increase blood flow and promote heat loss through the skin. Conversely, when the body is too cold, blood vessels constrict (vasoconstriction) to reduce heat loss.
- Sweating: When the body is too hot, sweat glands release sweat, which evaporates and cools the body.
- Shivering: When the body is too cold, muscles contract involuntarily, causing shivering. This generates heat.
- Behavioral Responses: The body can also regulate temperature through behavioral responses, such as seeking shade or wearing warm clothing.
Blood Sugar Control
The body also carefully regulates blood sugar levels. Blood sugar, or glucose, is a vital source of energy for cells. However, excessive or insufficient blood sugar levels can have serious consequences.
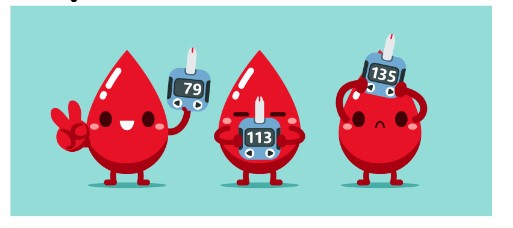
The pancreas, a gland located near the small intestine, plays a crucial role in blood sugar control. It produces two hormones: insulin and glucagon.
- Insulin: When blood sugar rises after a meal, the pancreas releases insulin. Insulin stimulates cells to take up glucose from the bloodstream, lowering blood sugar levels.
- Glucagon: When blood sugar falls, the pancreas releases glucagon. Glucagon stimulates the breakdown of glycogen, a stored form of glucose, in the liver. This releases glucose into the bloodstream, raising blood sugar levels.
The body's ability to regulate blood sugar levels is essential for preventing conditions such as diabetes and hypoglycemia.
Fluid Balance
Maintaining fluid balance is essential for many bodily functions, including regulating blood pressure, maintaining electrolyte levels, and supporting kidney function.
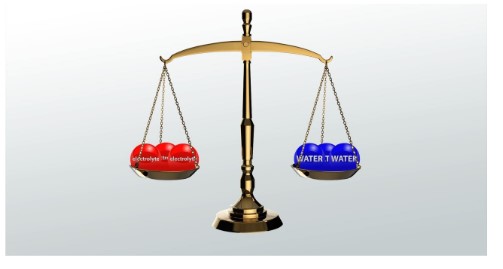
The kidneys play a crucial role in regulating fluid balance. They filter blood, reabsorbing water and electrolytes as needed. Hormones also help to control fluid balance
- Aldosterone: This hormone, produced by the adrenal glands, stimulates the kidneys to reabsorb sodium and water, increasing blood volume and blood pressure.
- Antidiuretic Hormone (ADH): ADH, also produced by the hypothalamus, stimulates the kidneys to reabsorb water, increasing blood volume.
When the body is dehydrated, the kidneys reduce water loss and increase thirst. Conversely, when the body has excess fluid, the kidneys increase water excretion.
Section 3: Homeostasis and Health
When homeostasis is disrupted, it can lead to a variety of health problems. These conditions can range from mild to severe and can affect multiple systems in the body.
Common Health Issues Associated with Homeostatic Imbalance
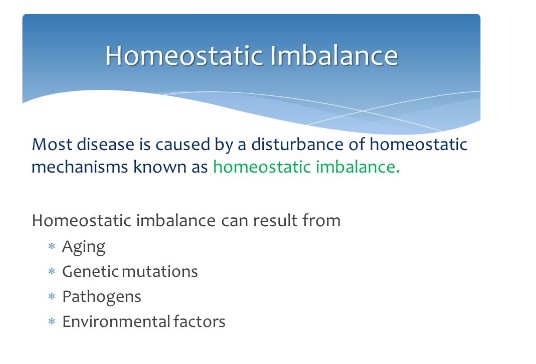
- Diabetes: Diabetes is a condition characterized by high blood sugar levels due to a deficiency or resistance to insulin. Insulin is a hormone produced by the pancreas that helps regulate blood sugar levels. When homeostasis is disrupted and blood sugar levels become too high, it can lead to a range of complications, including heart disease, stroke, kidney disease, and nerve damage.
- Dehydration: Dehydration occurs when the body loses too much fluid and cannot adequately replenish it. This can happen due to excessive sweating, vomiting, diarrhea, or inadequate fluid intake. Dehydration can lead to fatigue, dizziness, headache, and even kidney stones.
- Hypertension: Hypertension, or high blood pressure, is a condition characterized by elevated blood pressure. It can be caused by a variety of factors, including hormonal imbalances, kidney disease, and lifestyle factors. High blood pressure can increase the risk of heart disease, stroke, and kidney disease.
- Hypothyroidism: Hypothyroidism is a condition in which the thyroid gland does not produce enough thyroid hormone. This can lead to a variety of symptoms, including fatigue, weight gain, cold intolerance, and constipation.
- Hyperthyroidism: Hyperthyroidism is a condition in which the thyroid gland produces too much thyroid hormone. This can lead to symptoms such as weight loss, rapid heartbeat, nervousness, and heat intolerance
Recognizing Signs of Homeostatic Imbalance
- Fatigue: Feeling tired and exhausted, even after getting enough sleep.
- Thirst: Excessive thirst, especially when you're not physically active.
- Dizziness: Feeling lightheaded or dizzy
- Rapid heartbeat: A heart rate that is faster than normal.
- Changes in appetite: Increased or decreased appetite.
- Weight gain or loss: Unexplained weight gain or loss.
- Frequent urination: Need to urinate more often than usual.
- Constipation or diarrhea: Changes in bowel habits.
- Cold intolerance or heat intolerance: Difficulty tolerating cold or hot temperatures.
- Joint pain or stiffness: Aches and pains in the joints.
If you experience any of these symptoms, it's important to see a healthcare provider for evaluation. Early diagnosis and treatment can help prevent serious complications.
Seeking Medical Attention
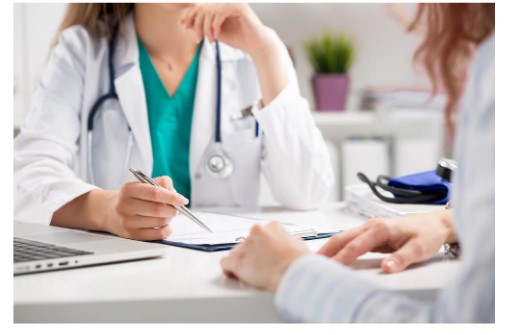
If you notice any signs or symptoms of homeostatic imbalance, it's essential to seek medical attention. A healthcare provider can diagnose the underlying cause and recommend appropriate treatment.
During your appointment, your doctor may ask about your medical history, symptoms, and lifestyle. They may also conduct a physical examination and order blood tests or other diagnostic tests.
Once a diagnosis is made, your doctor can develop a treatment plan to address the underlying condition and restore homeostasis. Treatment may involve lifestyle changes, medications, or other interventions.
By recognizing the signs of homeostatic imbalance and seeking medical attention when necessary, you can help to prevent serious health problems and maintain your overall well-being.
Section 4: Tips for Supporting Homeostasis
While the body is remarkably adept at maintaining homeostasis, certain lifestyle choices can help to support this vital process. By making conscious decisions about your diet, exercise, hydration, stress management, and healthcare, you can optimize your body's ability to maintain a stable internal environment.
Healthy Diet
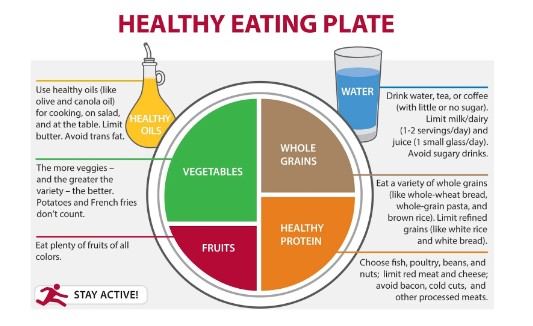
- Fruits and Vegetables: These are rich in vitamins, minerals, and antioxidants, which are essential for various bodily functions. Aim for at least five servings of fruits and vegetables per day.
- Whole Grains: Whole grains, such as brown rice, quinoa, and whole-wheat bread, provide fiber, vitamins, and minerals. Fiber helps regulate digestion and can contribute to weight management.
- Lean Proteins: Protein is essential for building and repairing tissues. Choose lean sources of protein, such as poultry, fish, beans, and lentils.
- Healthy Fats: Healthy fats, such as those found in avocados, nuts, and seeds, are essential for cell function and hormone production.
- Limit Processed Foods: Processed foods are often high in unhealthy fats, added sugars, and sodium. These can contribute to weight gain, high blood pressure, and other health problems.
A healthy diet can help to regulate blood sugar levels, maintain a healthy weight, and support overall well-being.
Regular Exercise

Physical activity is essential for maintaining homeostasis. It helps to improve circulation, strengthen muscles, and maintain a healthy weight. Regular exercise can also help to reduce stress, improve mood, and boost energy levels.
Aim for at least 30 minutes of moderate-intensity exercise most days of the week. This could include walking, running, swimming, cycling, or dancing.
Adequate Hydration

Staying hydrated is crucial for maintaining fluid balance and supporting various bodily functions. Dehydration can lead to fatigue, dizziness, headache, and other health problems.
The amount of water you need to drink each day will vary depending on factors such as your activity level, climate, and overall health. A good general guideline is to aim for at least eight glasses of water per day.
Stress Management

Chronic stress can disrupt homeostasis and contribute to a variety of health problems. Effective stress management techniques can help to reduce stress and promote relaxation. These include:
- Meditation: Meditation involves focusing on the present moment and calming the mind. There are many different types of meditation techniques, such as mindfulness meditation and guided imagery.
- Yoga: Yoga combines physical postures, breathing exercises, and meditation to promote relaxation and reduce stress.
- Deep Breathing: Deep breathing exercises can help to slow down your heart rate, lower blood pressure, and reduce stress.
- Time Management: Effective time management can help to reduce stress by preventing feelings of being overwhelmed.
- Social Support: Spending time with loved ones and connecting with others can provide emotional support and reduce stress.
Regular Check-ups

Regular medical check-ups can help to identify potential health issues early on and support overall well-being. These check-ups should include:
- Annual Physical Exams: A physical exam can help to assess your overall health and identify any potential problems.
- Regular Screenings: Regular screenings for conditions such as high blood pressure, diabetes, and cancer are important for early detection and treatment.
- Dental Check-ups: Regular dental check-ups are essential for maintaining oral health and preventing dental problems.
By making conscious choices about your lifestyle and seeking regular medical care, you can help to support homeostasis and optimize your overall health and well-being.
Conclusion
Homeostasis is a complex process that underlies our health and well-being. It is the body's ability to maintain a stable internal environment, despite external changes. This delicate balancing act is essential for optimal cell function, disease prevention, enhanced performance, and stress resilience.
By understanding the science behind homeostasis, we can appreciate the complexity and beauty of human biology. We can also make informed choices to support this vital process.
Reflecting on Your Lifestyle
Take a moment to reflect on your own lifestyle choices. How do your eating habits, exercise routine, stress management techniques, and healthcare practices impact your body's ability to maintain homeostasis? Are there areas where you could make improvements?
Small changes can have a significant impact on your overall health and well-being. By incorporating healthy habits into your daily life, you can help to optimize your body's ability to maintain homeostasis.
Additional Resources
If you're interested in learning more about homeostasis, there are many resources available. Here are a few suggestions:
- Books:
- The Human Body by David Suzuki
- The Body's Balancing Act by David Linden
- Websites:
- National Institutes of Health (NIH): https://www.nih.gov/
- American Physiological Society: https://www.physiology.org/
These resources can provide valuable information about the science of homeostasis and practical tips for supporting this vital process.
By understanding homeostasis and taking proactive steps to support it, you can improve your overall health and well-being. Remember, your body is a remarkable machine that works tirelessly to maintain balance. By providing it with the support it needs, you can help it to thrive.
Interactive Elements
- Quiz: Test your knowledge of homeostasis with a short quiz.
- Infographic: Visualize the key concepts of homeostasis with an informative infographic.
Guides
- Benefits of Protein
- 7 Healthy Eating Habits
- 7 Most Effective Exercises At Home
- Home Workout Plan Without Equipment
- Top 10 Biggest Nutrition Myths
- How To Get Flexible Body?
- Weight Loss VS Fat Loss
- What is Keto Diet?
- What Is Minerals?
- What Is Digital Marketing ?
- Best Free Tools For Beginner You Tubers
- Best Teas For Weight Loss & Fat Burning
- Green Tea: Health Benefits And Side Effects
- Yoga for Weight Loss and Fat Burning
- What Is Type-2 Diabetes?
- How To Write Eye-Grabbing Resume
- The Ultimate Guide To Prepare For An Interview
- 10 Best Health Benefits Of Eating Mango
- healthy eating habits for kids
- 10 tips for starting your Fitness Transformation
- 10 Reasons Why People Hate Gym & How to Overcome Them
- Fuel Your Passion For Nutrition: Explore The Power Of A Nutrition Course
- Shed Pounds with Ease: Vegetarian Diet Plan for Weight Loss Revealed!
- Anabolic steroids: Types, Uses, and Side Effects
- Find Your Path to Success: Choosing the Right Fitness Certification Program in India
- learn gym trainer course offline at surat with best faculties
- Learn about Body Composition and How it Affects Your Health
- Nutrition course online with affordable fees
- Online Dietitian Plan vs In-Person Consultation: Which is Right for You?
- The Importance Of Fitness Education In Today's World


About Dr.Gautam Jani
Dr. Gautam is a civil engineer. By passion he is a dietitian and had started practising it in the year 2016. He is the founder of fitnesswithgomzi firm established in 2018. He has achieved many certificate from ACSM, ISSA and VLCC.

